Think of a scenario where a new diagnostic tool is developed. Doctors are excited about its potential. Yet, before integrating it into routine care, they must ensure its reliability and accuracy. This is where clinical validation becomes vital. This practice safeguards against errors and inconsistencies in patient care.
Clinical validation verifies that every medical claim and diagnosis aligns with actual patient conditions. It’s not just about ticking boxes but about upholding the standards of medical accuracy and patient safety.
What is Clinical Validation?
Clinical validation is an essential process in healthcare that ensures the accuracy of medical records. It involves reviewing and confirming that the clinical evidence backs diagnoses and procedures documented in health records. This process is integral in maintaining the integrity of patient data.
The Process of Clinical Validation
Clinical validation begins with a thorough examination of a patient’s medical record. Healthcare professionals scrutinize the documented information. They then compare it against clinical indicators and patient history evidence.
They verify whether the diagnoses and procedures are clinically substantiated. Beyond cross-checking data, this validation is evaluated against established medical standards and practices.
Importance of Clinical Validation
Clinical validation plays an essential role in healthcare compliance and quality assurance. It ensures that medical records accurately reflect the patient’s clinical condition, necessary for meeting regulatory standards and providing high-quality care.
Accurate documentation through clinical validation helps healthcare organizations maintain compliance with laws and regulations, thereby avoiding legal and financial penalties. Moreover, clinical validation significantly impacts healthcare reimbursement and audits. Reimbursements from insurance providers, including Medicare and Medicaid, depend heavily on accurate and complete medical documentation.
In the context of audits, clinical validation acts as a preemptive measure. It reduces the risk of audit failures by ensuring that all claims and documentation are accurate and compliant. This rigorous validation process helps healthcare facilities avoid costly penalties and maintain their reputation.
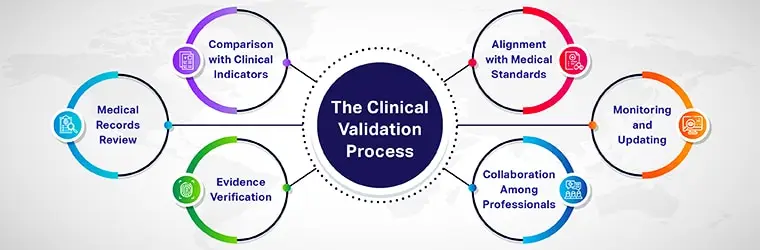
The Clinical Validation Process
The clinical validation process is a systematic approach in healthcare to ensure the accuracy and legitimacy of medical records. This process involves several key steps:
- Review of medical records: Healthcare professionals thoroughly review the patient’s medical history.
- Comparison against clinical indicators: They compare the documented diagnoses and procedures against clinical indicators and medical benchmarks.
- Evidence verification: The process includes verifying that clinical evidence supports each documented diagnosis and procedure.
- Alignment with medical standards: The diagnoses and procedures are checked to ensure they align with accepted medical standards and practices.
- Collaboration among professionals: Clinical documentation integrity specialists, coding professionals, and healthcare providers collaborate in this process.
- Continuous monitoring and updating: The process involves ongoing monitoring and updating of records to maintain accuracy and compliance.
These steps ensure that medical records accurately reflect the patient’s clinical status. This is crucial for quality patient care, healthcare compliance, and proper reimbursement practices.
Challenges in Clinical Validation
Clinical validation, while essential in healthcare, presents several challenges that can impact its effectiveness:
- Complexity of medical data: Deciphering complex medical data and matching it with clinical evidence can be challenging.
- Variability in clinical standards: Differences in clinical standards and practices can lead to inconsistencies in validation.
- Inadequate training: Healthcare professionals may lack adequate training in the latest clinical validation techniques.
- Time constraints: Time pressures in a busy healthcare setting can hinder thorough clinical validation.
- Data privacy concerns: Ensuring patient data privacy while conducting validation is a constant challenge.
- Resistance to change: There may be resistance from healthcare staff to adopt new validation processes or technologies.
Failure to conduct proper clinical validation can lead to misdiagnoses, incorrect treatments, and issues with healthcare compliance. This can result in reduced patient care quality, potential legal ramifications, and financial penalties for healthcare organizations.
Therefore, overcoming these challenges is critical for the accuracy and reliability of medical records and the overall effectiveness of healthcare delivery.
Best Practices in Clinical Validation
Effective clinical validation is key to maintaining high standards in healthcare documentation. Implementing best practices ensures accuracy and compliance in medical records.
- Develop and implement clear guidelines for clinical validation processes.
- Provide ongoing training for healthcare professionals on the latest validation techniques and standards.
- Leverage technology to aid in the validation process to ensure efficiency and accuracy.
- Apply clinical standards consistently across all validations.
- Establish and enforce internal criteria and policies for clinical validation to ensure uniformity.
- Involve a multidisciplinary team. It must include clinicians and coding professionals in the validation process.
- Conduct regular audits of clinical warranties and provide feedback for continuous improvement.
- Keep abreast of changes in healthcare regulations and standards impacting clinical validation.
Adhering to these best practices can significantly enhance the effectiveness of clinical validation.
The Future of Clinical Validation

As healthcare embraces digital transformation, clinical validation will increasingly rely on sophisticated algorithms and AI to handle complex data. These advancements promise to streamline the process. They make it more adaptive to the dynamic nature of healthcare while maintaining stringent standards of accuracy and compliance.
Conclusion
Clinical validation is a critical component in healthcare. It ensures the accuracy and integrity of medical records. It involves a meticulous process of verifying diagnoses and procedures against clinical evidence.
As the medical field continues to evolve, clinical validation adapts too. It integrates technology to enhance efficiency and accuracy. This practice safeguards healthcare standards and significantly contributes to the overall quality and safety of patient care.